Parkinson’s disease is a common neurodegenerative disease, affecting more than 2% of people over 75, with estimated 7 to 10 million affected people worldwide. Although traditionally Parkinson’s disease (PD) is thought of as a disorder of movement, with tremor and slowing of movement being the cardinal features, it can cause a wide range of other non-motor symptoms and frequently leads to dementia. These non-motor symptoms, are common, can occur even before motor symptoms become evident and are often the most troubling for patients.
Visual hallucinations, the sensation of seeing objects that are not really there, are a common non-motor symptoms in PD, affecting up to 70% of individuals over the course of the disease. As well as causing distress, visual hallucinations have a significant impact on the quality of life of patients and their families: hallucinations often herald the cognitive decline and are a strong predictor for nursing home placement.
The wide variety of visual hallucinations
The experience of visual hallucinations vary from person to person and can change across the course of the disease. Commonly, people with Parkinson’s disease experience one or more of the following hallucinations:
- Passage hallucinations: where a person, animal or indefinite object is seen briefly passing in the periphery of the vision. Patients usually describe these moving forward from behind “in the corner of their eye” and they are usually accompanied by a strong urge to look towards the illusory image.
- Illusions: where a real object is briefly misperceived as something else (for example, mistakenly thinking that a pile of clothes on the floor is a dog). A specific type of visual illusion that is commonly seen in PD is pareidolia; this is the illusory perception of faces of people or animals from irrelevant visual stimuli (for example seeing a face out of a complex geometrical pattern in a wallpaper). Pareidolia can also happen in healthy people and has been used by artists; a famous example can be seen in Figure 1. Another common illusion in Parkinson’s is kinetopsia, where stationary objects are seen as moving.
- Presence hallucinations: A feeling of presence of someone nearby (a person or animal other than one’s self). This is often not recognised as a specific person although it can be sometimes identified as a relative or friend.
- Complex visual hallucinations: These almost invariably involve people and animals, often in vivid detail, with patients describing scenes of elaborately dressed Victorian women or small children playing. Although they can occur at any time and place, visual hallucinations often happen in the evening and usually in the patient’s own home.


Earlier in the disease course, hallucinations are more commonly minor, with passage hallucinations and illusions. These are usually short-lasting for only few seconds, occur more than once a week, and are rarely distressing. As the disease progresses, people start to experience more complex hallucinations, which can be extremely detailed and well-formed. Hallucinations in other sensory modalities can also occur but these are usually less well-formed, for example muffled sounds, touches or smells.
Initially, people can often recognise that the experienced hallucinations are not real; they have preserved insight. As the disease progresses, insight may become lost and hallucinations can lead to false beliefs or delusions: for example, believing that a hallucination of a man in the house at night is a thief.
Visual hallucinations are challenging to treat
Despite their impact to patients and carers, treatment options for hallucinations are limited, with anti-psychotic medications most commonly prescribed. In Parkinson’s disease, this poses an important challenge as antipsychotic medications can be associated with worse cognitive deterioration and increased risk of stroke and death in elderly people. So treating hallucinations in people with Parkinson’s disease may actually accelerate their cognitive impairment.
For this reason, the first step in treating hallucinations in Parkinson’s is to investigate and treat coexisting infections or reduce medications that could be causing or worsening hallucinations. Treatments for motor symptoms of Parkinson’s disease are common antagonists of visual hallucinations, which poses an additional challenge. Finding a balance between treating the motor symptoms and treating hallucinations can be very difficult and adding an antipsychotic medication is often necessary despite their risk.
More recently, a different category of medications that affect the receptors for serotonin (a chemical in the brain which is involved in mood, learning and memory), have been identified as a potential drug treatment. One of these medications, Pimavanserin, recently showed to improve psychosis and visual hallucinations in Parkinson’s disease, particularly those with poorer cognition in a large randomised trial. Another such medication is ondansetron, which is already widely used as an anti-sickness medication. Ondansetron showed improvement in Parkinson’s-associated hallucinations in small studies but further studies are currently underway to evaluate its effectiveness.
A better understanding of hallucinations is needed
Finding treatments for hallucinations that are both effective and safe is an area of great unmet need. But to find effective treatments, a greater understanding of hallucinations is first needed. Due to their transient nature, visual hallucinations can be challenging to study and no clear mechanism has been found. However recent models suggest that visual hallucinations in Parkinson’s are related to a shift in the balance of different brain networks.
In recent years it has become more apparent that different brain regions are not independent from each other but are related and influence one another by forming networks: different regions are physically connected (forming structural networks), are activated simultaneously (functional networks) or can be thought of as parts of the same influences or pathways when we are trying to make a decision about the world (computational networks). The balance of different functional brain networks is disrupted in patients with Parkinson’s disease who experience visual hallucinations. These are patterns of brain activation that can be traced using resting state functional MRI. Specifically networks that are related to attention and perception seem to be less active and one network which is normally active during rest and mind-wandering, the default mode network (DMN) seems to be overactive in people with Parkinson’s disease.
Computational networks (the different influences and pathways that affect how we perceive things) also show imbalance in people with Parkinson’s disease and visual hallucinations. In recent years it has become more apparent that vision is an active rather than a passive process, with each person perceiving a visual object or scene in a slightly different way, taking into account their prior knowledge, expectations and experiences. This active visual perception, results in slightly different experiences amongst individuals and may explain why some people see Figure 1 as a duck and others as a rabbit, even though they are looking at the same object. In people with visual hallucinations, the integration of visual information with prior knowledge may be less effective leading to false images or hallucinations.

In our research group, we have recently showed that patients with Parkinson’s disease who hallucinate rely more on their prior knowledge compared with those that do not experience hallucinations (Figure 3). At the same time people with Parkinson’s and hallucinations show changes at the back of the eyes, the retina, and are less effective in accumulating visual information. In this way, hallucinations arise due to over-interpretation of visual input, or relying more heavily on prior knowledge.
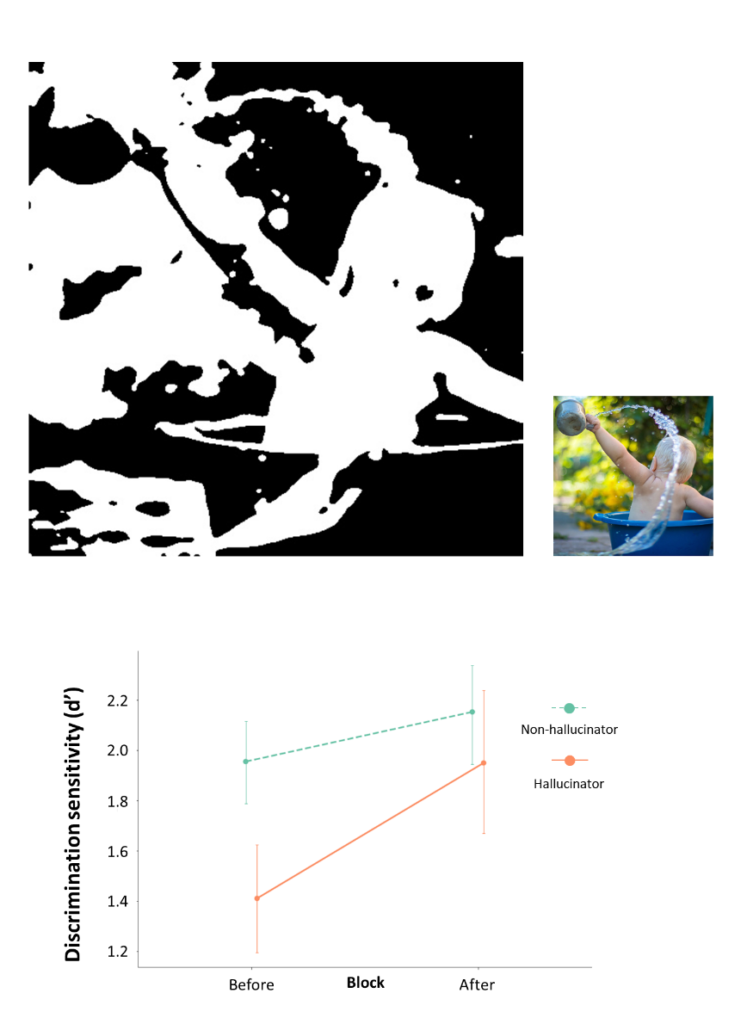
Top left: A two-tone image that is difficult to disambiguate without prior knowledge. This image was shown to people with and without Parkinson’s disease and they were asked to say whether it contains a person or not. This was repeated after seeing the template coloured image (top right).
Bottom: People with Parkinson’s and hallucinations improved much more than those without hallucinations after seeing the coloured figures.
Adapted from Zarkali A, Adams RA, Psarras S, Leyland LA, Rees G, Weil RS. Increased weighting on prior knowledge in Lewy body-associated visual hallucinations. Brain Commun. 2019;1(1):fcz007. doi:10.1093/braincomms/fcz007
Understanding the drivers and key brain regions in shifting network control is a key area of ongoing research that might help us better understand and treat visual hallucinations. More and more researchers are now focusing on gaining a better understanding the interactions between networks and how we can influence the relative balance between them. This approach opens new possibilities for therapeutic options and may also help us improve existing treatments for Parkinson’s disease. For example, using imaging with a network rather than a region approach, researchers were able to better predict which patients with Parkinson’s will develop side effects when treated with deep brain stimulation (which involves surgically implanting wires directly into the brain). Similar network-based approaches might help us better understand why hallucinations happen in Parkinson’s and how we can effectively treat them without having to compromise the management of other symptoms such as movement.

Angelika Zarkali is a specialist registrar in Neurology with an interest in cognitive neurology and movement disorders. Her clinical and research interest is the aetiology, diagnosis and treatment of Parkinson’s disease dementia and Dementia with Lewy Bodies. After gaining clinical experience at UCLH, East Kent and St George’s hospitals, Angelika joined the Dementia Research Centre, funded by an Alzheimer’s Research UK Fellowship and supervised by Dr Rimona Weil and Professor Geraint Rees. Her research aims to shed light on the neural correlates of visual hallucinations in Parkinson’s disease and Dementia with Lewy Bodies. Specifically, Angelika is trying to understand the changes in brain structure in patients who have hallucinations and what effect these structural changes have on brain function and behaviour.




