There are pervasive gender inequalities in modifiable risk factors for dementia, which place women at a disadvantage throughout the life course. Further, gender and socioeconomic inequalities intersect, rendering women more vulnerable to the detrimental health effects of poverty and deprivation. A successful prevention strategy for dementia must reflect a thorough understanding and a strong commitment to reducing gender inequalities in exposure to risk factors throughout the life course.
In the absence of a disease modifying treatment, prevention remains the most powerful tool available to effectively address the challenge of dementia and to reduce its enormous impact on individuals, families and communities around the world. But evidence on the enormous potential of reducing the risk of dementia is constantly growing. While age is the biggest risk factor for dementia, many other risk factors contribute to increasing the likelihood of developing the disease. When such factors can be altered through environmental and behavioural change – i.e. are modifiable (Fig. 1), they offer an opportunity to significantly decrease or delay the risk of developing dementia.
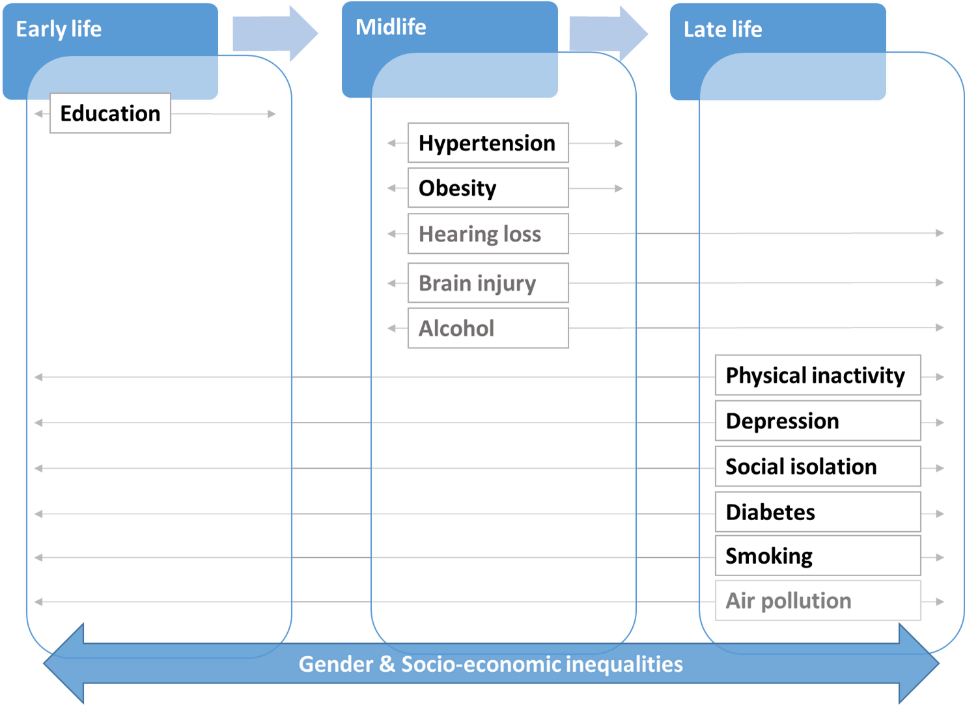
Most potentially modifiable risk factors exhibit strong socio-economic inequalities. Among people with lower income/wealth and lower educational attainment the prevalence of risk factors is considerably higher. Recent evidence is increasingly revealing a pronounced sex- and gender-dimension to many of the same risk factors. At the intersection of gender and socioeconomic inequalities, growing numbers of women find themselves at increased risk of dementia, with limited support to mitigate it.
Gender and socio-economic inequalities in clinical depression
To take but one example, the prevalence of depression, throughout the life course, presents a pronounced gender gap. Everywhere data is available, women more frequently experience depression over the life course and are more susceptible to it in older age (OECD/EU, 2018). As a result, the burden of depression and its economic, social and health related consequences are disproportionately borne by women. At the same time, depression is more common in people with lower socio-economic status, be it measured by education level, income or wealth. In Europe, the poorest groups are more than twice as likely to report chronic depression as those at the top of the income distribution. Such income inequalities are more pronounced among women suggesting they are more vulnerable to the detrimental mental health effects of poverty and deprivation (Fig. 2).
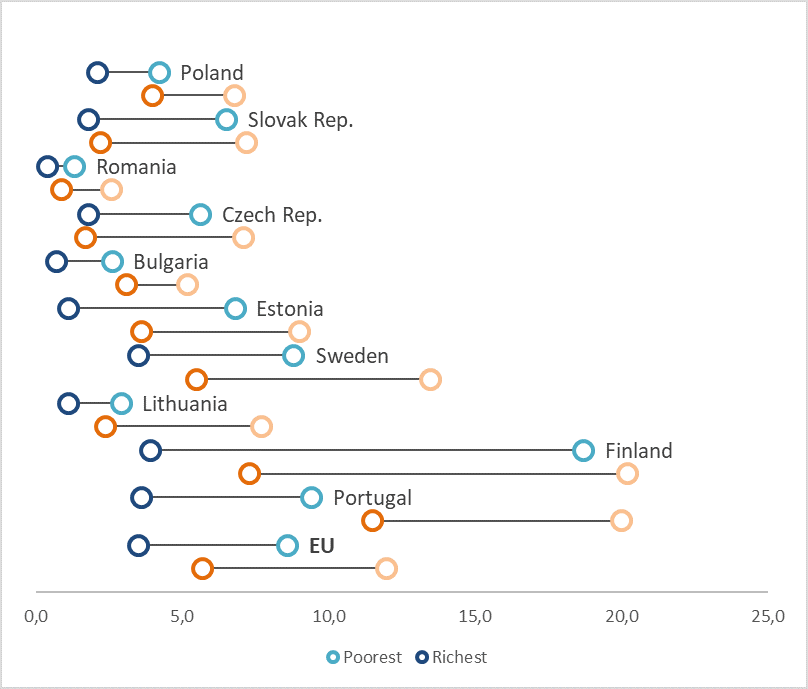
Note: Based on data from the Eurostat Database, as reported in Health at a Glance: Europe 2018. The richest group refers to people in the top income quintile (the 20% of the population with the highest income), while the poorest group refers to people in the bottom income quintile (the 20% of the population with the lowest income).
Depression and dementia are the two most common mental and neurological disorders among older individuals at a global level and account for a considerable proportion of years lived with disability in this age group (WHO, 2017). By reducing the prevalence of depression in the general population and particularly among vulnerable groups (i.e. older women, lower income), significant gains in health-related quality of life, as well as reductions in dementia risk can be achieved.
Gender equity at the core of dementia prevention strategies
The marked gender differences in the prevalence of dementia are often explained by the survival advantage of women. It is true that in the oldest age group (85+) where dementia prevalence is highest, women outnumber men 2 to 1. However, evidence is building for a complementary, although not competing, explanation: there are pervasive inequalities in risk factors which systematically place certain population groups, including women, at increased age-adjusted risk of dementia. While this is cause for alarm, it also suggests a pathway to the prevention of dementia worldwide.
A successful prevention strategy for dementia must take a population health approach and be built on reducing gender inequalities in risk factors and access to treatment and care. Such an approach can use purposive targeting of preventive health programs to women and lower socioeconomic groups or of sustained action to increase accessibility and availability of high-quality care. Equally important is for prevention strategies to take a life-course approach, beginning in early life and helping to prevent gender and socioeconomic inequalities in health from developing in the first place. Progress can be and has been made! Gender-based inequalities in educational attainment have been reduced considerably over recent decades and will likely contribute to reducing the number of dementia cases for future cohorts of older women. If similar gains were to be achieved across all modifiable risk factors, millions of dementia cases could be prevented across the world.

Stefania Ilinca, PhD. is senior researcher at the European Centre for Social Welfare Policy and Research in Vienna. She works at the interface between policy and research, dividing her time between applied research, policy advice and advocacy efforts with a focus on long-term care, equity, health and social policy.
Disclaimer
The material presented here is based on Ilinca S. & Suzuki E. (forthcoming July 2021) Gender and socio-economic differences in modifiable risk factors for Alzheimer’s disease and other types of dementia throughout the life course.
In: Ferretti, Santuccione Chada & Schumacher (Eds.) Sex and Gender Differences in Alzheimer’s Disease. Elsevier.
References
Livingston, G., Huntley, J., Sommerlad, A., Ames, D., Ballard, C., Banerjee, S., et al. (2020). Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. The Lancet, 396(10248), 413-446
Sindi, S., Mangialasche, F., & Kivipelto, M. (2015). Advances in the prevention of Alzheimer’s Disease. F1000prime reports, 7
World Health Organization. (2017 b). Mental health of older adults. Factsheets. World Health Organization. Available at: https://www.who.int/news-room/fact-sheets/detail/mental-health-of-older-adults
OECD/EU (2018), Health at a Glance: Europe 2018: State of Health in the EU Cycle, OECD Publishing, Paris. Available at: https://doi.org/10.1787/health_glance_eur-2018-4-en.