Dr Clare Walton from Alzheimer’s Society in the UK and a member of the WYLD Steering group reflects on her experiences at the ADPD 2017 conference held in Vienna from 29th March to 2nd April.
Alzheimer’s and Parkinson’s Disease (ADPD) Congress happens every two years bringing together over 3,000 researchers from the field of neurodegeneration working on Alzheimer’s or Parkinson’s but also on Parkinson’s disease dementia, Lewy body dementia, frontotemporal dementia and other rarer conditions. Bringing these research fields together to share their latest findings makes a lot of sense from a clinical perspective. Although we define each of these forms of dementia as different conditions, we are increasingly learning about the overlaps between them.
Several speakers, including Dr Lauren Walker from the University of Newcastle, reported that it is common to find the biological hallmarks of more than one kind of dementia present in the same person. These hallmarks can be seen in brain tissue after death and, more recently, in living people using new brain imaging techniques.
Perhaps unsurprisingly people who show signs of more than one type of dementia experience a faster decline in cognitive function. These findings have important implications for the treatment of people with dementia. For example, the presence of amyloid plaques in the brains of people with Dementia with Lewy bodies means we should be considering whether they can benefit from the anti-amyloid treatments that are currently in development for people with Alzheimer’s disease.
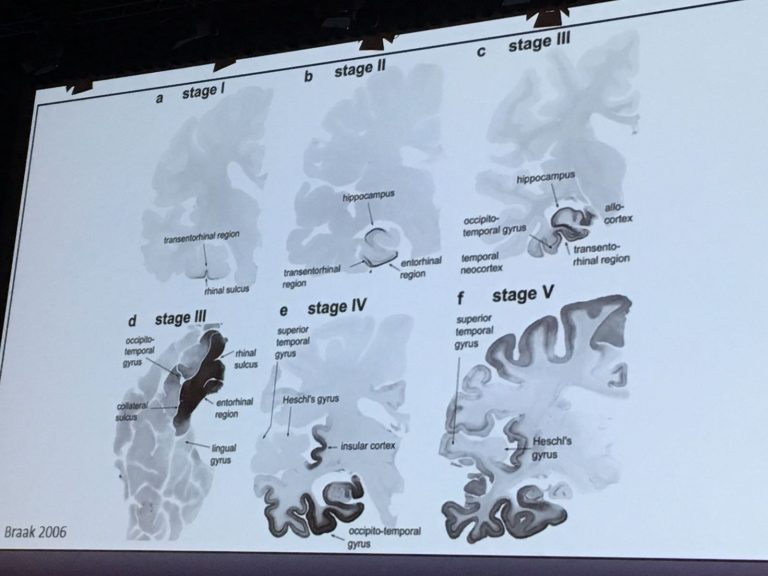
Several sessions at the conference focused on disease processes that are shared by more than one condition. A topic I find intriguing is the spreading of damaged toxic proteins between brain cells, which has been observed in Parkinson’s, Dementia with Lewy bodies and in Alzheimer’s disease. In the first two conditions, the protein alpha-synuclein is the culprit. In Alzheimer’s it is the tau protein that passes between interconnected brain regions, seemingly bringing about the damage of brain cells as it spreads.

Tau spreading was first discovered in 2009 and since then it has been observed in cells in a dish, in animal models and in the brains of people with dementia. Importantly, in people with Alzheimer’s disease, the movement of toxic tau from the entorhinal cortex to the rest of the brain correlates with the development and progression of dementia symptoms. This discovery opens up a whole new avenue for developing treatments.
One approach being explored is to use antibodies to mop up tau after it has been released by damaged brain cells. Researchers hope this will reduce how much tau spreads across the rest of the brain and might slow down cognitive decline. The first vaccine against tau has been tested for safety and is currently being tested for beneficial effects in people with mild to moderate Alzheimer’s disease.
Abnormal tau protein is also a hallmark of frontotemporal dementia (FTD), a condition that currently has no treatments. Data presented by AXON Neuroscience at ADPD 2017 showed that their Alzheimer’s tau vaccine can trigger the production of useful antibodies in people with FTD. Later in 2017 they will begin a clinical trial of the vaccine in people with a specific kind of FTD called Primary Progressive Aphasia.
This was my first time at the ADPD Congress and I was curious to learn how the two different research
fields would come together. There was clearly an expanse of common ground in terms of the research techniques being developed and the molecular pathways and cellular mechanisms being explored. It was encouraging to see researchers working on one condition learn from the successes and failures of those working in a related disease area. I have no doubt that this cooperative approach will speed up the progress being made for people living with all of these neurodegenerative conditions.